Researchers develop treatment model for HIV / AIDS and depression
With a shortage of mental health professionals, an international team has trained nurses to treat clinically depressed HIV-positive people in South Africa.
Today, people living with HIV / AIDS can stay healthy if they are able to follow routine care and take drugs that reduce their virus to undetectable levels. But for people living with HIV who also struggle with depression, it is often an insurmountable challenge, especially in South Africa, which has the highest number of cases in the world and a significant shortage of mental health professionals. .
But a new study published in the Journal of the International AIDS Society has local and global implications for successfully treating mental health and HIV / AIDS in settings like South Africa or even Miami, the epicenter of new cases. in the USA.
In the study, an international team of researchers, led by Steven Safren of the University of Miami and two colleagues, demonstrated the effectiveness of training nurses in public HIV clinics to deliver cognitive behavioral therapy ( CBT) specially adapted to help people with depression and uncontrolled disorders. HIV adhere to their prescribed drug regimen. CBT is a proven approach to changing erroneous or unnecessary thought or behavior patterns.
“We know that treating HIV-positive people who are clinically depressed with antidepressants alone does not affect their viral load. Their depression may improve, but not their adherence, ”said Safren, professor of psychology and director of the University’s Center for HIV / AIDS and Mental Health Research. “So, given the global shortage of mental health professionals, we have shown that it is possible to train nurses to provide cognitive behavioral therapy for adherence and depression (CBT-AD), an intervention which successfully treats both clinical depression and uncontrolled HIV. “
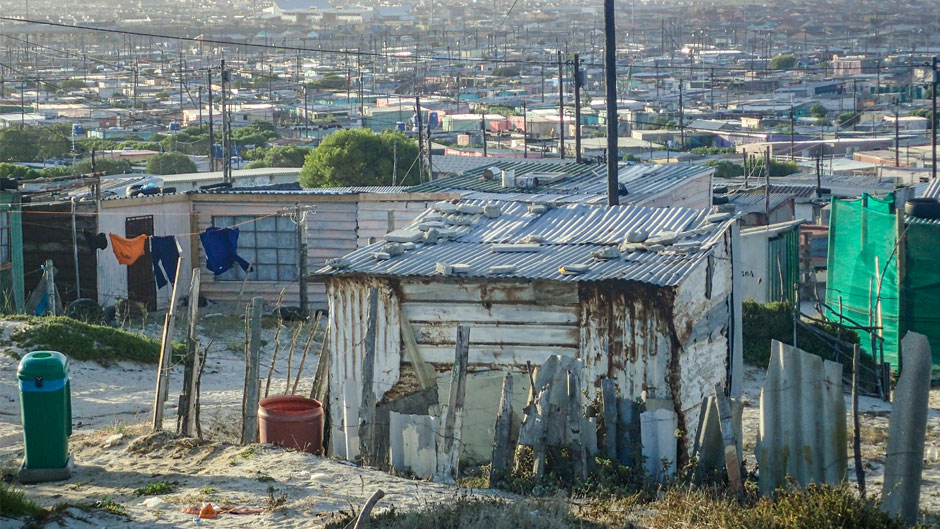
Safren, who joined the University in 2015 from Harvard Medical School, conducted the study in a poor suburb just outside Cape Town, South Africa, with fellow researchers John A. Joska, director of the HIV Mental Health Research Unit and Professor of Psychiatry at the University of Cape Town, and Conall O’Cleirigh, Associate Professor of Psychology at Harvard and Director of Behavioral Medicine at Massachusetts General Hospital.
For their study, the researchers recruited 161 patients with uncontrolled HIV / AIDS and clinical depression from four public health clinics in Khayelitsha Township. Although a doctor can prescribe antidepressants to patients, clinics have limited psychological services, like the country in general. According to the study, South Africa has only 0.28 psychiatrists and 0.32 psychologists per 100,000 population.
At the start of the study, all participants received the usual enhanced care for clinically depressed HIV-AIDS patients who did not achieve viral suppression after receiving the first month of their antiretroviral medication. This usual treatment included another prescription and follow-up meetings with an adherence counselor.
But half of the patients were also randomly assigned to eight CBT-AD sessions, in which specially trained nurses integrated depression treatment strategies with adherence counseling including life skills modules, depression, relaxation, mood monitoring and problem solving.
The idea, Safren said, was to help patients “turn down the volume” of their mental health symptoms, so that they would be more open to advice on the benefits of taking their medications. To track their adherence, patients also received an electronic pill box which, each time it was opened, transmitted a real-time signal to a web server.
And, according to the researchers, the task-sharing approach offered by nurses has proven to be effective. Patients who completed CBT-AD sessions were more than 2.5 times more likely to achieve undetectable viral loads than those who received usual care.
Now, Safren noted, the next step will be for the research team to assess how to sustainably implement the CBT-AD approach in South Africa, if not South Florida. He said the task-shared approach might be viable in Miami, where there are fewer services to help people achieve viral suppression than in other U.S. cities with large populations of people living with the virus.
“South Africa has the most HIV / AIDS cases in the world and Miami is the city with the highest incidence of new cases in the United States, so there is a parallel,” said Safren. “And unlike places like New York or Massachusetts, where people are more likely to be virally deleted, Florida doesn’t have the same public health resources. If, for example, you are an HIV positive patient at Massachusetts General or Fenway Health, where I previously worked, and you miss your visit, or your viral load gets out of hand, social workers will step in and help. It doesn’t happen as often in Florida and other places in the United States with less public health funding for HIV / AIDS.
In addition to Safren, Joska, and O’Cleirigh, other study co-authors included Jasper S. Lee, a Ph.D. student, and Sierra A. Bainter, assistant professor, both in the Department of Psychology at the ‘University; as well as researchers from the University of Maryland, College Park; Mbarara University of Science and Technology, Uganda; the University of Washington in Seattle; and the University of Stellenbosch in Stellenbosch, South Africa.
Comments are closed.