 DePaul University Counseling Services made its first full-time hire of the school year. Two more full-time counselors will begin work in May 2022, according to UCS director Tow Yau. UCS plans to have a total of nine full-time board positions by June and will begin seeing students in fall 2022, according to Yau. These are […]]]>
DePaul University Counseling Services made its first full-time hire of the school year. Two more full-time counselors will begin work in May 2022, according to UCS director Tow Yau. UCS plans to have a total of nine full-time board positions by June and will begin seeing students in fall 2022, according to Yau. These are […]]]>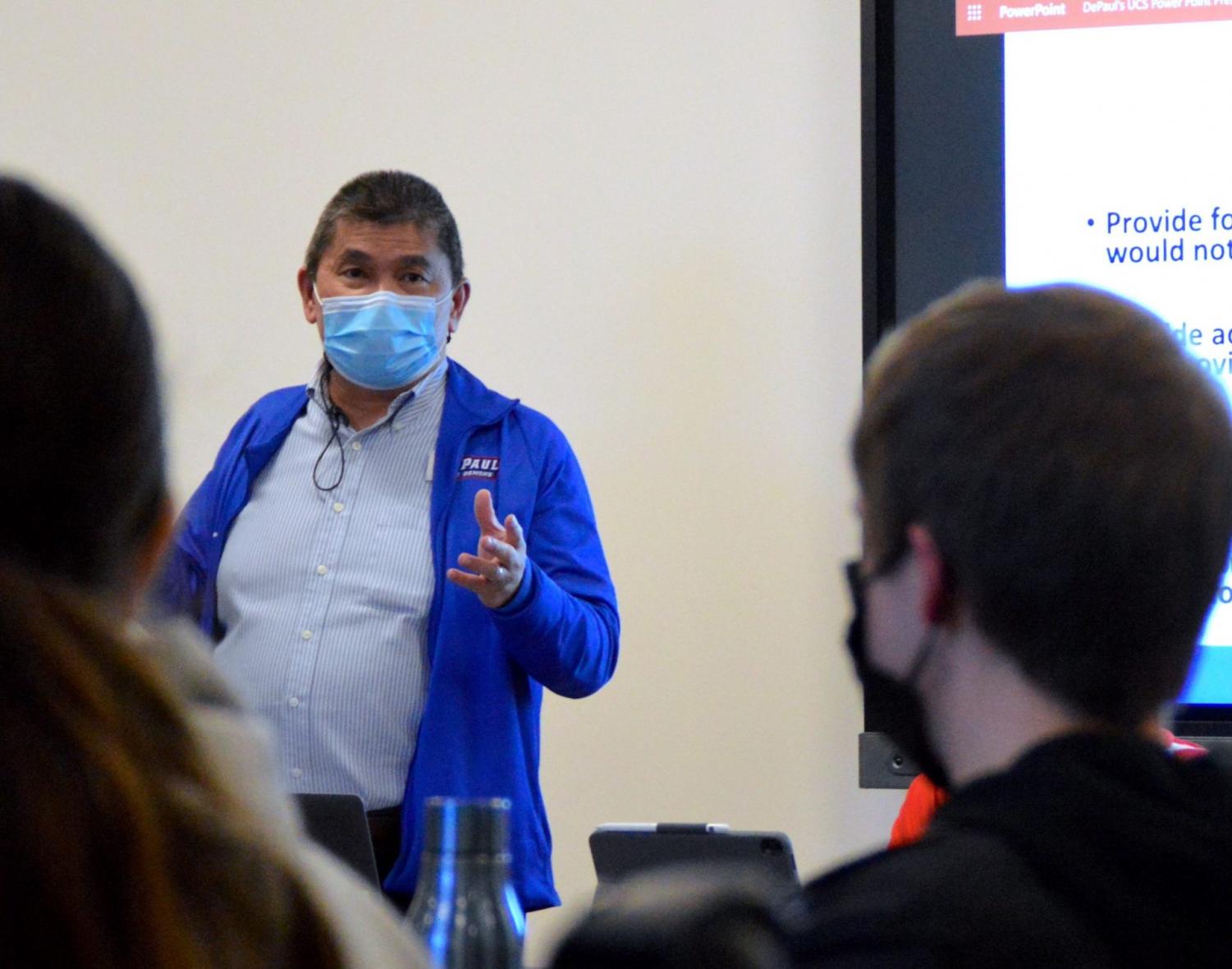
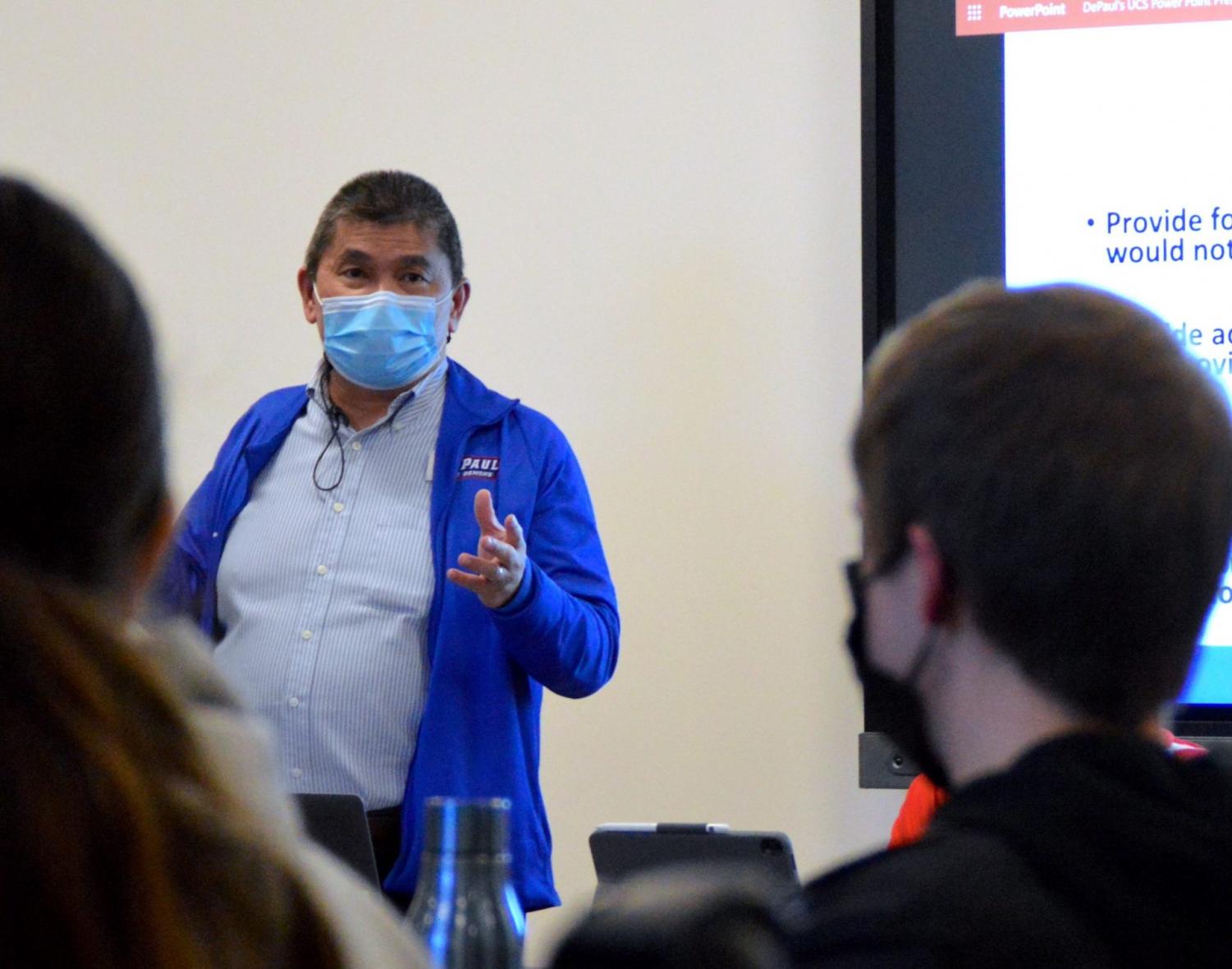
DePaul University Counseling Services made its first full-time hire of the school year.
Two more full-time counselors will begin work in May 2022, according to UCS director Tow Yau.
UCS plans to have a total of nine full-time board positions by June and will begin seeing students in fall 2022, according to Yau.
These are the first formal full-time hires made by UCS since outsourcing all counseling to My Student Support Program (SSP) in July 2021. Four temporary part-time counselors were hired in January and provided 15 hours of clinical services in Lincoln Park. and five to the loop, according to Yau.
“We have other applicants and hope to fill all remaining positions by June, although hiring in this area continues to be a challenge nationwide,” Yau said in a statement to The DePaulia.
Yau also confirmed that he continues to work with the Student Government Association (SGA) to create a mental health task force.
Riley Reed, SGA Senator for LGBTQ+ Students, said she heard student concerns about My SSP and the services available from the university. The working group is still in its planning phase.
“We as students want to make sure people have access to proper mental health care on college campuses because frankly, as we’ve seen since the pandemic, it’s been poor,” said Reed.
Students may encounter insurance issues if they choose to outsource counseling. During the fall term, UCS would make custom referrals based on insurance plans, according to Yau.
“Students are so frustrated because if you don’t like having certain insurance, it’s really hard to get covered,” Reed said.
DePaul students will have access to My SSP until the end of the academic year, according to Yau, and it is undetermined whether this will be renewed. Yau said students’ use of My SSP wavered throughout the term.
“The number of students accessing My SSP has decreased slightly but remains stable,” he said. “In our experience, the number of students accessing the app fluctuates throughout the term.”
Sophomore Evelyn Hernandez said she was referred to My SSP but was confused as to how it worked.
“It wasn’t clear how to set up an appointment; there wasn’t much explanation about it and it was difficult to navigate the website to figure out how to get an appointment in the first place,” Hernandez noted.
She attended three sessions with two different counsellors.
“I’ve had two sessions with my current counselor, and it’s been fine, but I also feel weird talking to a robot, but it’s been helpful,” Hernandez said.
My SSP says it is a phone, app and web based telehealth service, according to its home page. This term, DePaul students had the opportunity to meet their advisors in person.
“My SSP counselors in Chicago also hosted 30 in-person sessions with DePaul students,” Yau said.
The Division of Student Affairs hosted a Mental Health Fair this past term, where Courtney James, Director of Student Engagement, shared how different departments are trying to help students during UCS’s restructuring.
“We all know what’s going on with UCS,” James said in a previous DePaulia post. “It’s not the only solution. This is part of what students are asking for and what we need to do.
Senior management has not issued a statement regarding UCS. During the fall term, Vice President of Student Affairs Gene Zdziarski sent a college-wide email about My SSP, but didn’t explain why they added the resource. President A. Gabriel Esteban did not address the lack of counselors in his 2021 State of the University presentation.
Provost Salma Ghanem said at the joint university town hall between staff, faculty council and SGA in January that they “will assess the situation as it unfolds”, according to previous reports from The DePaulia. She also said that they have no plans to invest more funds in UCS.
“Once the positions at UCS are filled, the university will assess whether the needs for mental health services have been met,” Ghanem told the meeting.
There have been no updates since then from the administration about UCS.
“The upper administration must be held accountable for the lack of support they gave to their students,” Reed said. “They didn’t address it because they think [My SSP is] working. They need to be held accountable by the students as a whole because it doesn’t work.
UCS was also present at the mental health fair. Yau said it was a way to be more in tune with students’ mental health requirements.
“These events have reinforced how important it is for us to be attuned to the diverse mental health needs of our students,” Yau said. “It will be helpful to listen to students and learn about gaps in support as well as the types of services that would support student success. »
Reed said she trusts Yau to lead UCS and implement new programs for students. This includes hiring various advisors.
“[Yau] said he really wanted a fairer approach to [counseling] and getting therapists who really represent the student body, whether it’s gay therapists or therapists of color, those who can communicate a little better with students,” Reed said.
UCS plans to implement group treatment programs for alcohol and drug use, trauma-informed care, and survivors of sexual violence in the fall of 2022.
 During the troubling times of COVID, teens and young adults in Fort Bragg now have one more resource to rely on. Blue Door, a community service offering free and confidential health care, is now offered at the JD Center next to Fort Bragg High School every Wednesday beginning at 1:00 p.m. Blue Door is a […]]]>
During the troubling times of COVID, teens and young adults in Fort Bragg now have one more resource to rely on. Blue Door, a community service offering free and confidential health care, is now offered at the JD Center next to Fort Bragg High School every Wednesday beginning at 1:00 p.m. Blue Door is a […]]]>
During the troubling times of COVID, teens and young adults in Fort Bragg now have one more resource to rely on. Blue Door, a community service offering free and confidential health care, is now offered at the JD Center next to Fort Bragg High School every Wednesday beginning at 1:00 p.m. Blue Door is a program of Mendocino Coast Clinics, the local community health center whose mission is to build a healthy community by providing quality patient-centered health care to all coastal residents. Blue Door’s confidential services include birth control information, supplies, and behavioral health counseling. Blue Door’s expansion is part of the district’s ongoing effort to ensure students are as safe and supported as possible. Blue Door began to respond to an expressed need for accessible and confidential health care for teens and young adults. “It started as a community collaboration, and it continues to be a community collaboration,” said Stacy Pollina, reproductive health program manager at Mendocino Coast Clinics.
Blue Door’s expansion means even more growth potential. “Blue Door is part of the JD Center’s overall plan to be a hub that connects families to the resources they need,” Pollina said. On their first day of operation, Kei Velazquez, one of Blue Door’s medical providers, described his vision: “We want the process to be seamless: someone can be seen by a medical provider, talk to a counsel and participate in interactive art projects. We want to provide a safe space that offers tools to build self-esteem. Soon, Blue Door will offer family advocates, including the two recently hired bilingual liaisons by FBUSD, to help connect families with the support and services they need, such as food stamps and MediCal.”The new location makes it all possible,” Pollina said. “We’re excited to make Blue Door and its associated resources even more accessible to young people and their families.”
The entrance to the new Blue Door location has what you would expect of a clinic: a check-in counter, chairs to sit on while you wait. There are also a few rooms for exams or counseling sessions. However, to the right is a room you might not expect – a large room lit by two skylights on the high ceiling, an open door to let in a swath of sunshine and fresh air, and ornate walls of artwork created by a range of age groups in the community. Blue Door has partnered with FLOCKworks, a local non-profit organization supporting local collaborative arts initiatives, to create an inspiring and heartwarming space. “We hope to one day offer art workshops in this room, maybe even classes like sewing,” Velazquez said. “If nothing else, Blue Door will always be a safe place for teens and young adults.”
 Residents and families of Victoria will soon have better access to day-to-day primary health care services with the opening of the new Luther Court Community Health Center (CHC). Services will begin on Wednesday, March 16, 2022, prior to the completion of the CHC expansion and renovation. Work is underway to create 260 square meters (2,800 […]]]>
Residents and families of Victoria will soon have better access to day-to-day primary health care services with the opening of the new Luther Court Community Health Center (CHC). Services will begin on Wednesday, March 16, 2022, prior to the completion of the CHC expansion and renovation. Work is underway to create 260 square meters (2,800 […]]]>
Residents and families of Victoria will soon have better access to day-to-day primary health care services with the opening of the new Luther Court Community Health Center (CHC).
Services will begin on Wednesday, March 16, 2022, prior to the completion of the CHC expansion and renovation.
Work is underway to create 260 square meters (2,800 square feet) of purpose-built clinical space at Luther Court’s current location at 1525 Cedar Hill Cross Rd. The center is expected to open in June 2022 and operate at full capacity. by 2024-25.
The Luther Court CHC team will initially expand to include a doctor and three nurses who will begin tethering patients and offering virtual appointments next week. Patients requiring in-person care will be able to receive services in a temporary off-site space. The expansion will also add more registered nurses and other allied health care providers to the team.
“We are delighted that the Luther Court Society is already beginning the work of connecting the people of Victoria to the health care services they need in preparation for the completion of the Community Health Center refurbishment,” said Adrian Dix, health Minister. “As the company adds a community health center to its existing services, residents will have one more place to go to get the daily health care they need closer to home.
Once the center opens at its main location, approximately nine additional full-time equivalent clinical health care providers will be recruited to join existing staff at Luther Court to provide comprehensive primary care services with an emphasis on older people and people living with mental health issues. and substance use conditions. The team will include family physicians, nurse practitioners, registered nurses, a licensed practical nurse, a mental health and addictions worker, a community health outreach worker, a dietitian and an occupational therapist.
In addition, approximately six full-time equivalent support staff, including a primary health care director, will assist the clinical care team in delivering health promotion and wellness services and increasing access to housing. intergenerational.
The center will begin by opening Monday through Thursday from 8 a.m. to 8 p.m., Friday from 8 a.m. to 4 p.m. and Saturday from 8 a.m. to 12 p.m.
The Government of British Columbia will provide more than $2.2 million in operating budget once the center reaches full capacity. The province also provided one-time funding of more than $2.1 million for renovation costs.
“We know that in Victoria it is often difficult for people to get the health care they need when they need it most,” said Rob Fleming, MPP for Victoria-Swan Lake. “To meet this challenge, the new Community Health Center is a crucial part of the government’s commitment to provide better and faster access to health care across the province.
“The people of Greater Victoria deserve high-quality, accessible health care and that’s why our government is working hard to create solutions that meet their needs,” said Murray Rankin, MPP for Oak Bay-Gordon Head. . “BC’s primary care strategy builds on the good work that community organizations like Luther Court are already doing and will help our families and seniors.
Community health centers are not-for-profit or cooperative health care organizations that provide integrated, people-centered services and programs that reflect the needs of the communities they serve.
Since 1979, the Luther Court Society has provided an innovative model of care to improve the quality of life for older adults by providing housing options, care services and community interaction. The company is known for helping seniors live and age in place, and offers a variety of programs such as long-term care and independent and assisted living services. An affordable intergenerational housing project is also planned.
The Luther Court Society has a long history of collaborating with local community groups and organizations, with post-secondary apprenticeship partners and is a member of several collectives such as the BC Association of Community Health Centres. Recognized as a local health centre, the expansion of Luther Court into a community health center will help increase access to primary care, health promotion and wellness services, further meeting the needs from the community.
The Luther Court CHC is a collaboration between the Department of Health, Island Health, the Victoria Division of Family Practice and the Luther Court Society and will provide comprehensive primary care services to the local community. It will be part of the Victoria Primary Care Network and will be governed, owned and operated by the Luther Court Society.
Fast facts:
- There are approximately 100 community health centers run by health authorities and 30 community health centers run by the community in British Columbia.
- These centers focus on the integration of services and programs in primary care, health promotion and community wellness, and the social determinants of health.
Learn more:
To learn more about the province’s primary care strategy, visit: https://news.gov.bc.ca/releases/2018PREM0034-001010
To learn more about the Luther Court Society, visit: https://luthercourt.org/
A backgrounder follows.
 Roundtable participants meet via Zoom on Thursday evening. The opioid crisis is closer to home than many realize in Snohomish County, and the impacts are being felt throughout the community. It was one of the takeaways from Thursday night’s virtual opioid roundtable hosted by the Verdant Health Commission. Verdant Health Commission Chairman of the Board, […]]]>
Roundtable participants meet via Zoom on Thursday evening. The opioid crisis is closer to home than many realize in Snohomish County, and the impacts are being felt throughout the community. It was one of the takeaways from Thursday night’s virtual opioid roundtable hosted by the Verdant Health Commission. Verdant Health Commission Chairman of the Board, […]]]>
The opioid crisis is closer to home than many realize in Snohomish County, and the impacts are being felt throughout the community. It was one of the takeaways from Thursday night’s virtual opioid roundtable hosted by the Verdant Health Commission.
Verdant Health Commission Chairman of the Board, Jim Distelhorst, opened the meeting by sharing a 17 minute video on opioid use in Snohomish County, where overdose deaths have increased 20-30% since 2020. In 2020 alone, 525 Snohomish County residents died from opioid overdoses. Yakima County is the only other county in Washington with more opioid-related deaths.
Opioid use is not only harmful to users, it also harms other members of the community. For example, according to the Centers for Disease Control, one in three police officers will be stuck by a used needle during their career.
Verdant based in Lynnwood (find out more about how it works and how it is funded here) funds a range of health-related initiatives and has also launched its own Needle Service Program (SSP), Distelhorst explained. The needle exchange program provides drug users with sterile injecting equipment, safe disposal of needles, access to health care, treatment, testing and support.
Distelhorst pointed out that Verdant Health does not distribute free needles, which leads to more needles being improperly discarded.
“People only get the number of needles they give back,” Distelhorst said.
This helps limit the number of needles in the community and ensure that as many needles as possible are properly disposed of, he said.
Verdant has also addressed the opioid issue by hosting Narcan training. Narcan is a nasal spray that, when administered, blocks the effects of an opioid overdose. In January, Verdant partnered with Molina Healthcare and Snohomish County Social Services to host three training sessions attended by over 75 community members.
As a result, “there are now 75 more people in our community trained to recognize the signs of an overdose and administer Narcan,” Distelhorst said. “Each participant received a Narcan kit to take home. Each kit contains two Narcan nasal sprays. This means that there are now another 150 of these Narcan nasal sprays circulating in the community.
Verdant plans to hold additional Narcan training sessions in the coming months.
Roundtable speaker Linda Grant, CEO of Evergreen Recovery Center, said there is a stereotype that only teenagers use opioids, when in fact they don’t.
“We need to broaden our thinking about how we approach this,” Grant said. “About 70% of opioid-related deaths are people over 30.”
Evergreen’s naturopathic doctor, Andrew Dzikowski, said the clinic has seen a significant increase in relapses since the start of the COVID-19 pandemic. However, he added that Evergreen strives to be a place where patients feel they can come back if they need additional help.
“One of the things we strive for is that whether you’ve relapsed or not or are recovering, we want to be a safe place where people feel they can come back, whatever their situation. , without any judgement,” he said. “And that’s what we do. We create a safe and protected space for people to come at all stages of recovery and all stages of life and to guide them to a safer environment with housing, counselling, therapy, medical care and a warm, loving touch.
After the video, a Q&A session was held to answer questions from the community.
Many commenters have asked where teens can get drug treatments and access programs like SSP.
Distelhorst said the Center for Human Services offers outpatient treatment for teens. The center is a non-profit, community-based youth and family services agency that provides counseling and promotes drug and alcohol prevention. Northpoint Recovery, located in Bellevue, also offers treatment for children ages 12 to 17 and accepts Medicaid.
Grant said she empathizes with young people trying to seek help for addictions as resources have dwindled in recent years.
“The treatment of young people has just gone down terribly in terms of resources,” she said. “I know our legislature is trying to reinforce that this time, but the Center for Human Services is about it. Even the inpatient facility, Sundown M Ranch [located in Yakima] is the last hospital treatment center for young people. It’s just dying for no really good reason.
A commenter asked if facilities are experiencing longer stays than before due to the presence of drugs with stronger trace amounts.
According to Mishelle Rutherford, director of health services at Evergreen, the average stay for patients in rehab is five days. However, stays are getting longer as many drugs are now mixed with fentanyl, a synthetic opioid that is 80 to 100 times more potent than morphine. Because fentanyl takes so long to leave the body, patients experience withdrawal symptoms for longer periods of time.
“We find that it lives in the fat cells,” she said. “So he comes out at different times. So someone can feel better one day in rehab, and the next day they’re back in full withdrawal. It was really difficult to manage. »
Another commenter linked to this question, asking if it was proving difficult to convince insurance companies to cover longer stays.
Rutherford said Evergreen hasn’t had too many problems with insurance companies so far.
“As long as we can show there’s a medical need for them to be there,” she said. “This is where it gets tricky, because what we might consider a medical need in our detox field may not be exactly what the insurance company considers a medical need. So that poses problems. »
In fact, Rutherford said, there are more problems with patients leaving early.
“We end up having a lot of people leaving against medical advice around day four or day five because they don’t feel better,” she said. “So it’s kind of a complicated room just to get them through full detox. And of course going through rehab: that’s just the very beginning.”

Distelhorst ended the meeting by thanking the community for joining in and being open to learning more about the complicated processes of addiction treatment.
Any other questions or comments can be sent to Zoe Reese at [email protected].
— by Lauren Reichenbach
 CrossOver Healthcare Ministry recently announced that it was among 49 recipients to receive a grant from Direct Relief’s Fund for Health Equity, which mobilizes financial resources for organizations focused on non-clinical interventions that affect a person’s health. Commonly referred to as the social determinants of health, these factors include an individual’s physical, social, political, cultural […]]]>
CrossOver Healthcare Ministry recently announced that it was among 49 recipients to receive a grant from Direct Relief’s Fund for Health Equity, which mobilizes financial resources for organizations focused on non-clinical interventions that affect a person’s health. Commonly referred to as the social determinants of health, these factors include an individual’s physical, social, political, cultural […]]]>
CrossOver Healthcare Ministry recently announced that it was among 49 recipients to receive a grant from Direct Relief’s Fund for Health Equity, which mobilizes financial resources for organizations focused on non-clinical interventions that affect a person’s health. Commonly referred to as the social determinants of health, these factors include an individual’s physical, social, political, cultural and economic environment.
The 49 organizations received funding for a wide range of initiatives, including a campaign to overcome anti-Asian hostility and its effects on well-being; an initiative to develop more active lifestyles among members of the Yurok tribe; a center supporting the welfare of black women; and an organization focused on improving birth outcomes for refugee populations, primarily from African and Asian countries.
CrossOver was awarded a $250,000 grant from the Health Equity Fund for its work to provide high-quality, compassionate health services to low-income, uninsured, and medically underserved residents of the Greater Richmond area . CrossOver provides a medical home for patients, offering innovative integration of healthcare services under one roof, including primary and specialty care, chronic disease management, medication, dental, vision, pediatrics, counseling , women’s health and OB, HIV/AIDS diagnosis and treatment, case management and health education.
Each year, CrossOver provides care to more than 6,200 clients. CrossOver patients come from very different backgrounds: 80% of patients do not speak English as their first language, and more than 62% of all patients list Spanish as their primary language.
“This general operating support grant makes the work of CrossOver possible,” said Julie Bilodeau, CEO of CrossOver. “Quality healthcare requires excellence at every level: staff, facilities, programs, patient support and more. We are very grateful for Direct Relief’s support of our mission to provide health care to those in need.
“This round of funding honors the organizations on the front lines of their communities who are already working tirelessly to eliminate health disparities,” said Byron Scott, Health Equity Fund Co-Chair and Board Director. director of Direct Relief and chairman of its medical board. Advice. “These funds will allow these exemplary organizations to pursue innovation while improving health outcomes for vulnerable populations in diverse communities across our country.
The winners were selected by the Advisory Board of the Health Equity Fund.
Thanks for the reading!
If you enjoy our content, please consider making a monetary contribution to help us keep our news free.
Click here to contribute!
 With the spring semester in full swing, the Taylor University Counseling Center has set up therapy groups and workshops for students and faculty. Three therapy groups will meet on a weekly basis for three or four weeks. Each will address a variety of topics, including healthy relationships, managing anxiety and stress, and trauma and resilience. […]]]>
With the spring semester in full swing, the Taylor University Counseling Center has set up therapy groups and workshops for students and faculty. Three therapy groups will meet on a weekly basis for three or four weeks. Each will address a variety of topics, including healthy relationships, managing anxiety and stress, and trauma and resilience. […]]]>
With the spring semester in full swing, the Taylor University Counseling Center has set up therapy groups and workshops for students and faculty.
Three therapy groups will meet on a weekly basis for three or four weeks. Each will address a variety of topics, including healthy relationships, managing anxiety and stress, and trauma and resilience.
Registration closed on February 14 for the Healthy Relationships and Trauma and Resilience groups, but registration for a second Anxiety and Stress Management section is open until this Friday, March 11.
There are approximately 25 people currently registered to participate in therapy groups.
Kathy Chamberlain, Director of the Counseling Center, started in July 2020. She has over 30 years of social work experience and specializes in anxiety, trauma work, couples work and mental disorders. ‘mood.
“I hope that one, people recognize that they are not alone and two, that they get the resources they need to make the changes they need,” Chamberlain said.
Like the therapy sessions, the counseling center will host three workshops this semester that students and faculty can attend without registering. The topics of the workshops are communication and conflict resolution, eating disorders and cognitive resetting.
Chamberlain said the counseling center tries to provide workshop opportunities once a month so the Taylor community can learn more about mental health.
The first of three, Communication and Conflict Resolution, met Feb. 15 from 4-5 p.m. in the Cornwall Auditorium to discuss practical communication skills and conflict resolution techniques needed in various relationship situations.
The Disordered Eating Workshop will take place on March 15 from 4-5 p.m. in Cornwall for faculty and staff and 6-7 p.m. in Alspaugh East for students. Members of Shelah House, an eating disorder treatment center in Anderson, Ind., will share their knowledge about early signs of the disorder, body image, and treatment options. Students participating in the second session are encouraged to bring their lunch to the space.
For the final Cognitive Reset workshop, there will be a session on April 12 from 4-5pm in Cornwall. This is specifically aimed at students, providing ways to identify negative thought patterns regarding self-esteem and ways to rewrite those beliefs in a positive light.
Freshman Jonathan Berry said he has been attending individual therapy sessions since the end of J-term and also attended the conflict resolution workshop.
“Even if you don’t get all of your problems resolved right now, it really helps to talk to someone like a professional,” Berry said. “It’s useful even if you’re just organizing your thoughts.”
As an added incentive for students, many professors offer extra credit for attending workshops due to their built-in educational component.
For example, Mike Guebert, professor of geology and environmental science, offered his students additional credit opportunities if they use the advice center and hand in a brief account of their experience.
The counseling center usually receives a quarter of the student population, whether it is a one-time appointment or ongoing appointments. However, Chamberlain said that by the end of 2021 their numbers had increased by 33%, approaching 60% usage of Taylor’s student body.
“The need for mental health care is greater than it has ever been,” Chamberlain said.
One of Chamberlain’s passions in mental health treatment is preventative care. Realizing the need for an outward-looking approach, Chamberlain said it is only now with the COVID-19 pandemic that mental health professionals have begun to intentionally practice preventive care.
Most topics for therapy groups and workshops came directly from student feedback in light of promoting preventive care. According to Chamberlain, communication and conflict resolution was the number one ask of Taylor students who completed a survey sent out through announcements late last fall.
“Our hope is that we reach people who aren’t already in our clinic,” Chamberlain said.
QR codes and counseling center fact sheets are available across campus for easy access. Additionally, grounding boxes—kits containing supplies designed to reduce stress and anxiety—can be found in each dorm as well as at the Academic Enrichment Center. Specifically, they include toys, coloring tools, and therapy lights that mimic sunlight.
Individual appointments can be booked by emailing [email protected] and walk-in sessions are open Monday through Friday at 3 p.m. on a first-come, first-served basis.
For times when students or faculty cannot use in-person services, Chamberlain pointed out that online resources such as breathing techniques and mindfulness videos are easily accessible anytime through the MyTaylor portal.
The counseling center has office hours Monday through Friday from 8:00 a.m. to 5:00 p.m. For program updates and mental health tips, follow them on Instagram @tucounseling.
 (CBS4) – As the crisis in Ukraine continues, experts say it is likely to affect our mental health more than we even care to believe. Members of a territorial defense unit watch as a car approaches their barricade after curfew on the outskirts of eastern Kyiv on March 6 in Kyiv, Ukraine. Russia is continuing […]]]>
(CBS4) – As the crisis in Ukraine continues, experts say it is likely to affect our mental health more than we even care to believe. Members of a territorial defense unit watch as a car approaches their barricade after curfew on the outskirts of eastern Kyiv on March 6 in Kyiv, Ukraine. Russia is continuing […]]]>
(CBS4) – As the crisis in Ukraine continues, experts say it is likely to affect our mental health more than we even care to believe.
Members of a territorial defense unit watch as a car approaches their barricade after curfew on the outskirts of eastern Kyiv on March 6 in Kyiv, Ukraine. Russia is continuing its assault on major Ukrainian cities, including the capital Kiev, more than a week after launching a full-scale invasion of the country. (Photo by Chris McGrath/Getty Images)
“It’s definitely going to have an impact on our health,” said Blake Fleet, clinical director of Chrysalis Continuing Care in Denver. “I know things like this that seem out of control, the feeling that the world is going to end, are definitely going to cause higher levels of depression.”
And this depression can be passed on to your child, because children feed on the emotions of adults. That’s why Fleet said self-care is key for parents and it’s encouraged to talk to your child about the ongoing war, especially if the child is his age.
“A child under 5, there’s really no reason to discuss this information,” Fleet said. “But as they get older, they’re probably going to be exposed to that anyway, so we’re having that conversation with them, with older kids, and kind of helping them understand and work through their feelings is hugely important. .”
Fleet told CBS4 that when parents approach conversation, they need to adapt the language and words to a level the child will understand.
“Let the child lead, ask ‘Have you heard what’s happening in Ukraine? Is this something you want to know more about? How do you feel about this? “, He said.
Fleet said there are many resources available to help with mental health issues like therapy and online services, but her big message for parents is to take care of themselves.
“We have to get help, reach out. The kids are going to feed off of us,” Fleet said. “So if they feel like we’re calm, relaxed and in control, they feel like they can do the same for themselves.”
The state of Colorado has a program called I Matter that offers three free counseling sessions for children ages 12-18.
 Caroline Miller suffered from anxiety and postpartum depression three years ago. Miller said she noticed signs and symptoms with her first child, but didn’t seek help until her second child was seven months old. “She [her doctor] started me on medication and referred me to the perinatal program,” she said. “When I got a call […]]]>
Caroline Miller suffered from anxiety and postpartum depression three years ago. Miller said she noticed signs and symptoms with her first child, but didn’t seek help until her second child was seven months old. “She [her doctor] started me on medication and referred me to the perinatal program,” she said. “When I got a call […]]]>
Caroline Miller suffered from anxiety and postpartum depression three years ago.
Miller said she noticed signs and symptoms with her first child, but didn’t seek help until her second child was seven months old.
“She [her doctor] started me on medication and referred me to the perinatal program,” she said. “When I got a call from them they said, well, I’m sorry to tell you, but our waiting list is six months and we only take people until by the time their baby is one year old.”
Miller decided to pay for therapy out of pocket and that’s when everything changed. She received neuro-linguistic programming and decided to become certified in therapy for herself.
She said working in the hospital during the pandemic was the catalyst that pushed her to qualify to help others.
“I love watching these people grow and flourish and I wish I had that when I was going through it,” Miller said.
In a statement to CTV News, HSN spokeswoman Krista Lennox-Fryd said referrals to the hospital’s perinatal mental health program have increased 29% over the past year.
“While our programs are making every effort to see people as soon as possible, due to a high volume of referrals, patients may be placed on a waitlist for services,” the statement said.
“The waiting list for the perinatal mental health program is currently two months. If mothers need support sooner, they can follow up with their primary health care provider or other community support programs.
Unni Kleppe, who was able to get help from the program, said it helped her immensely.
“I have to say that I was very proactive in getting help,” Kleppe said.
“If I didn’t hear from them I would call. When I was first turned down I spoke to my doctor straight away and she helped me. I really believe we We need to focus more on mental health care – like prenatal care – during pregnancy care and postnatal care because it’s hard to navigate.”
As a registered nurse, Miller said sometimes health benefits won’t cover the services she provides, but she hopes to implement a rolling fee scale so she can help as many people as possible.
 Caroline Miller suffered from anxiety and postpartum depression three years ago. Miller said she noticed signs and symptoms with her first child, but didn’t seek help until her second child was seven months old. “She [her doctor] started me on medication and referred me to the perinatal program,” she said. “When I got a call […]]]>
Caroline Miller suffered from anxiety and postpartum depression three years ago. Miller said she noticed signs and symptoms with her first child, but didn’t seek help until her second child was seven months old. “She [her doctor] started me on medication and referred me to the perinatal program,” she said. “When I got a call […]]]>
Caroline Miller suffered from anxiety and postpartum depression three years ago.
Miller said she noticed signs and symptoms with her first child, but didn’t seek help until her second child was seven months old.
“She [her doctor] started me on medication and referred me to the perinatal program,” she said. “When I got a call from them they said, well, I’m sorry to tell you, but our waiting list is six months and we only take people until by the time their baby is one year old.”
Miller decided to pay for therapy out of pocket and that’s when everything changed. She received neuro-linguistic programming and decided to become certified in therapy for herself.
She said working in the hospital during the pandemic was the catalyst that pushed her to qualify to help others.
“I love watching these people grow and flourish and I wish I had that when I was going through it,” Miller said.
In a statement to CTV News, HSN spokeswoman Krista Lennox-Fryd said referrals to the hospital’s perinatal mental health program have increased 29% over the past year.
“While our programs are making every effort to see people as soon as possible, due to a high volume of referrals, patients may be placed on a waitlist for services,” the statement said.
“The waiting list for the perinatal mental health program is currently two months. If mothers need support sooner, they can follow up with their primary health care provider or other community support programs.
Unni Kleppe, who was able to get help from the program, said it helped her immensely.
“I have to say that I was very proactive in getting help,” Kleppe said.
“If I didn’t hear from them I would call. When I was first turned down I spoke to my doctor straight away and she helped me. I really believe we We need to focus more on mental health care – like prenatal care – during pregnancy care and postnatal care because it’s hard to navigate.”
As a registered nurse, Miller said sometimes health benefits won’t cover the services she provides, but she hopes to implement a rolling fee scale so she can help as many people as possible.
 A proposal in the Legislative Assembly aims to address the shortage of nurses in Oregon, which has jeopardized the quality of care, advocates say. No less than 350,000 people are hospitalized each year in Oregon, 1.3 million are treated in the emergency room and 13 million are treated on an outpatient basis. Nurses are also […]]]>
A proposal in the Legislative Assembly aims to address the shortage of nurses in Oregon, which has jeopardized the quality of care, advocates say. No less than 350,000 people are hospitalized each year in Oregon, 1.3 million are treated in the emergency room and 13 million are treated on an outpatient basis. Nurses are also […]]]>
A proposal in the Legislative Assembly aims to address the shortage of nurses in Oregon, which has jeopardized the quality of care, advocates say.
No less than 350,000 people are hospitalized each year in Oregon, 1.3 million are treated in the emergency room and 13 million are treated on an outpatient basis.
Nurses are also essential for providing care in medical clinics and long-term care facilities.
Advocates say the lack of nurses can lead to errors and lower quality care.
House Bill 4003 aims to alleviate the shortage of nurses by allowing students to treat patients under the supervision of a registered nurse and perform other duties, giving enrollees more time to do their jobs. The proposal would create a trainee nurse license for students who have had at least one semester of nursing education and passed a skills test. Proponents say their presence would free up experienced nurses, giving them more time to ensure patients receive proper care.
“I think this could be a huge help for nurses, both in terms of education and practice,” said Jana Bitton, executive director of the Oregon Center for Nursing, which conducts research and advocates nurses’ interests, in an e-mail. “This opens up opportunities for workplaces to integrate trainee nurses into their staff, which could alleviate staffing shortages in some situations.”
The influential Oregon Nurses Association, which represents 13,000 of the 72,000 licensed registered nurses in Oregon, also supports the bill.
“It’s not a panacea, but it will provide an on-ramp to the nursing profession and add qualified students to the health care team,” said association spokesman Kevin Mealy. “Registered Trainee Nurses can gain invaluable hands-on experience while supporting patients and nurses at the bedside and behind the scenes.
The proposal was unanimously approved by the House Health Care Committee last week and has gone to the Joint Ways and Means Committee, which decides budget matters.
It’s not a panacea, but it will provide an on-ramp to the nursing profession and add qualified students to the health care team.
– Kevin Mealy, spokesperson for the Oregon Nurses Association
In addition to creating a new license, the bill would add nurses to a program that offers therapy sessions. The Oregon Wellness Program now offers free, confidential counseling sessions for physicians, physician assistants, nurse practitioners, podiatrists, and dentists. The House bill would be extend the program to registered nurses.
The program, which would cost an additional $700,000 to include nurses, offers eight free one-hour therapy sessions a year with professionals. The program is confidential, unlike employee assistance programs, and appointments are guaranteed within 72 hours.
Although employer insurance plans cover mental health treatment, there is usually a co-pay and it usually takes time to get an appointment.
Nursing educators like Bitton also support the bill because it would also expand the nursing pipeline. In 2018, the Oregon Department of Employment said the state would need to add 2,600 nurses a year to replace those leaving and fill new positions created by health care expansion. But in 2019, less than 1,600 new graduates entered the job market.
“Right now we are seeing a delay in graduation due to a lack of clinical support,” Rep. Rachel Prusak, D-Tualatin, said in a forum before the session began. Prusak was a nurse for 20 years and a nurse practitioner for 14 years.
As chair of the House Health Care Committee, she proposed the bill after meetings with nurses, hospital and long-term care administrators and nursing educators.
“I watched this very closely,” Prusak said. “It’s really personal to me.”
Idaho and Washington already have nurse trainee licenses. Prusak said establishing such a license in Oregon is an easy first step.
“It will be one of the many things we need to do moving forward,” Prusak said.
The proposal would allow schools to award students credit for clinical experience. It would also expand the types of facilities that can temporarily use out-of-state nurses and extend the length of time they are allowed to practice in Oregon from one month to three months.
The Oregon Association of Hospitals and Health Care Systems supports the bill, as does the Oregon Primary Care Association, which represents 34 clinics serving low-income Oregonians.
“HB 4003 is a bill that reflects Oregon’s ability to be a leader in health care, and we appreciate that it has clear and predictable steps to begin addressing the issue,” said Andi Easton, vice president of government affairs for the hospital association. written testimony. “We particularly appreciate the effort to provide a gateway to quickly employ non-resident RNs in good standing in other states to work temporarily in Oregon hospitals.”