 DePaul University Counseling Services made its first full-time hire of the school year. Two more full-time counselors will begin work in May 2022, according to UCS director Tow Yau. UCS plans to have a total of nine full-time board positions by June and will begin seeing students in fall 2022, according to Yau. These are […]]]>
DePaul University Counseling Services made its first full-time hire of the school year. Two more full-time counselors will begin work in May 2022, according to UCS director Tow Yau. UCS plans to have a total of nine full-time board positions by June and will begin seeing students in fall 2022, according to Yau. These are […]]]>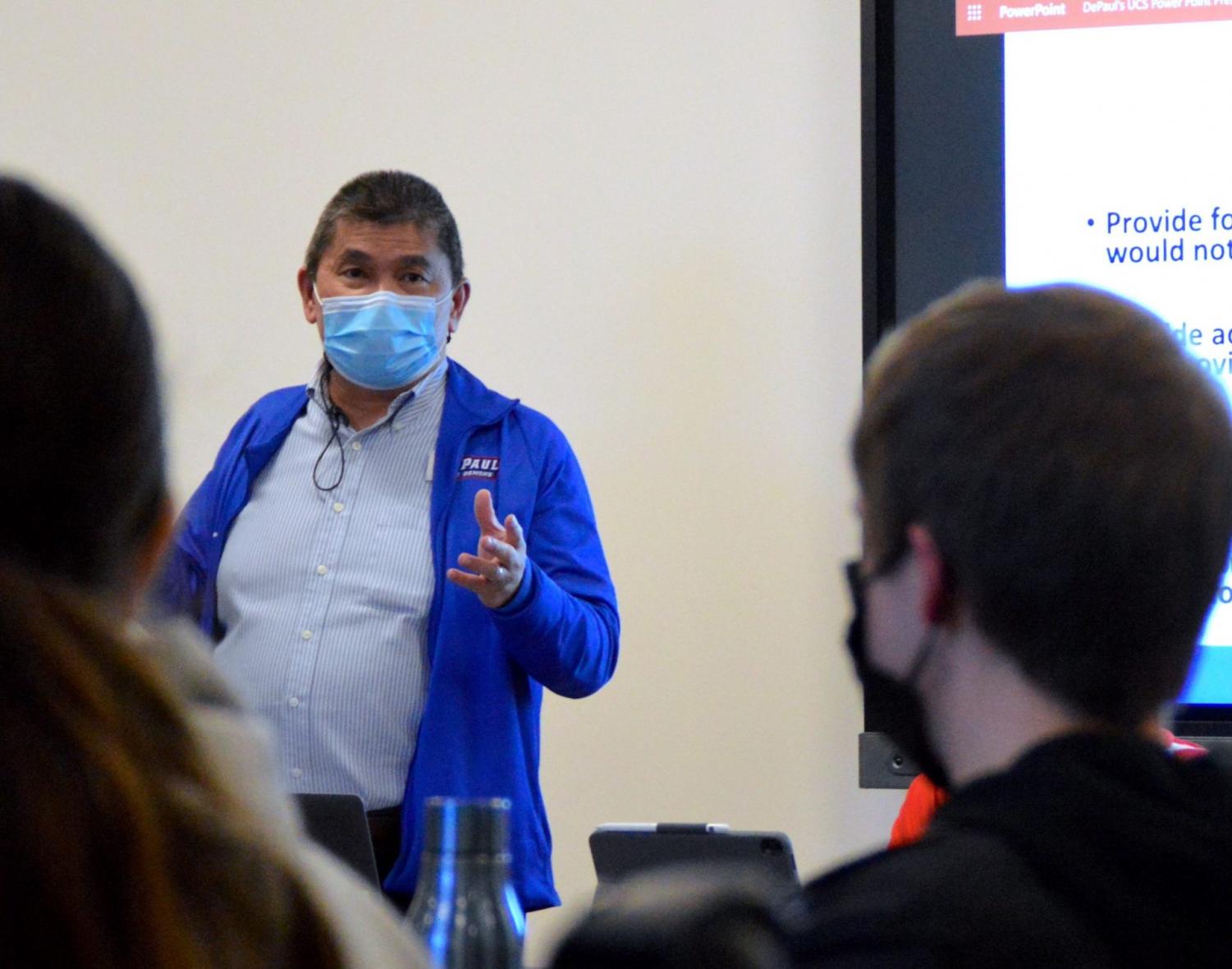
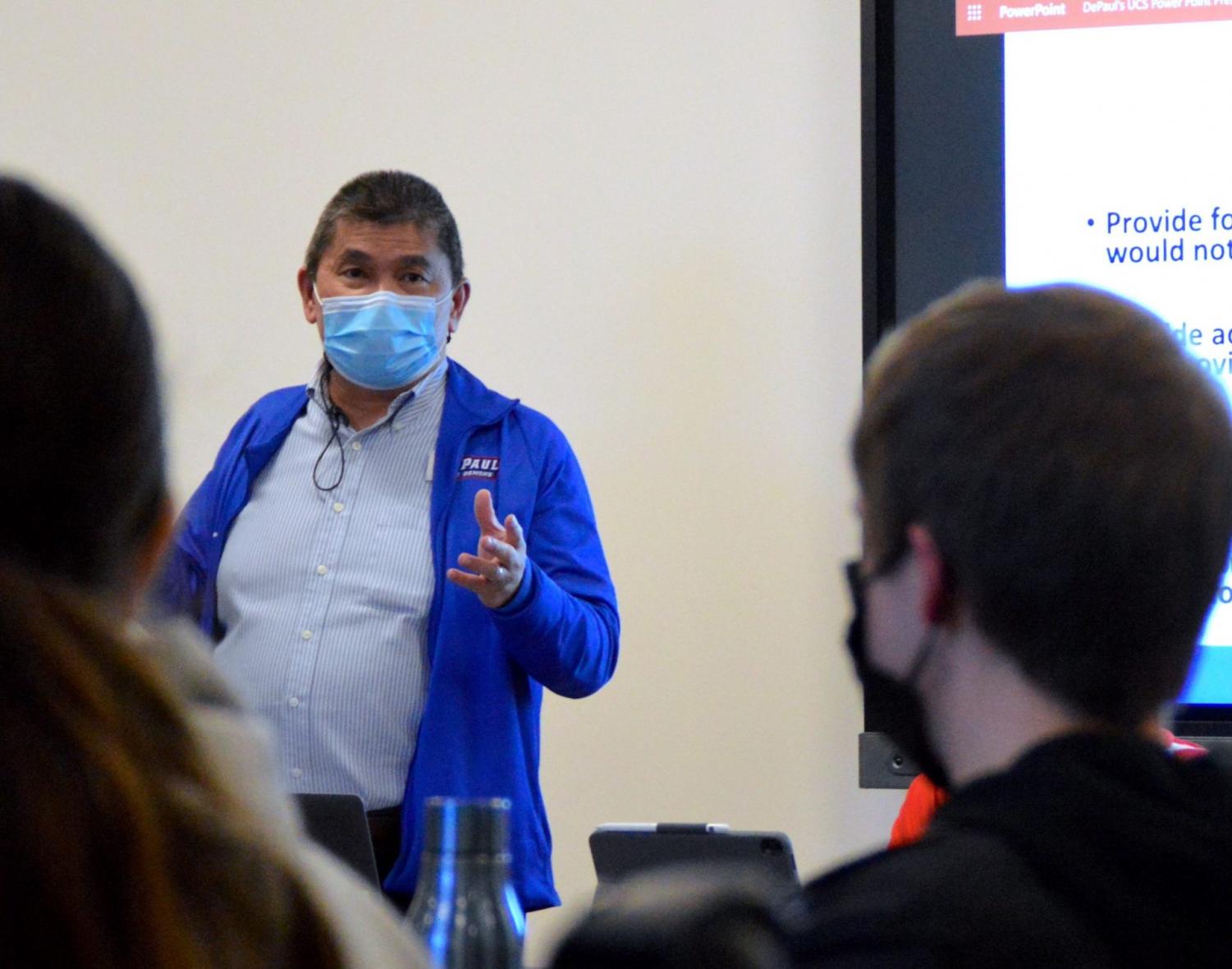
DePaul University Counseling Services made its first full-time hire of the school year.
Two more full-time counselors will begin work in May 2022, according to UCS director Tow Yau.
UCS plans to have a total of nine full-time board positions by June and will begin seeing students in fall 2022, according to Yau.
These are the first formal full-time hires made by UCS since outsourcing all counseling to My Student Support Program (SSP) in July 2021. Four temporary part-time counselors were hired in January and provided 15 hours of clinical services in Lincoln Park. and five to the loop, according to Yau.
“We have other applicants and hope to fill all remaining positions by June, although hiring in this area continues to be a challenge nationwide,” Yau said in a statement to The DePaulia.
Yau also confirmed that he continues to work with the Student Government Association (SGA) to create a mental health task force.
Riley Reed, SGA Senator for LGBTQ+ Students, said she heard student concerns about My SSP and the services available from the university. The working group is still in its planning phase.
“We as students want to make sure people have access to proper mental health care on college campuses because frankly, as we’ve seen since the pandemic, it’s been poor,” said Reed.
Students may encounter insurance issues if they choose to outsource counseling. During the fall term, UCS would make custom referrals based on insurance plans, according to Yau.
“Students are so frustrated because if you don’t like having certain insurance, it’s really hard to get covered,” Reed said.
DePaul students will have access to My SSP until the end of the academic year, according to Yau, and it is undetermined whether this will be renewed. Yau said students’ use of My SSP wavered throughout the term.
“The number of students accessing My SSP has decreased slightly but remains stable,” he said. “In our experience, the number of students accessing the app fluctuates throughout the term.”
Sophomore Evelyn Hernandez said she was referred to My SSP but was confused as to how it worked.
“It wasn’t clear how to set up an appointment; there wasn’t much explanation about it and it was difficult to navigate the website to figure out how to get an appointment in the first place,” Hernandez noted.
She attended three sessions with two different counsellors.
“I’ve had two sessions with my current counselor, and it’s been fine, but I also feel weird talking to a robot, but it’s been helpful,” Hernandez said.
My SSP says it is a phone, app and web based telehealth service, according to its home page. This term, DePaul students had the opportunity to meet their advisors in person.
“My SSP counselors in Chicago also hosted 30 in-person sessions with DePaul students,” Yau said.
The Division of Student Affairs hosted a Mental Health Fair this past term, where Courtney James, Director of Student Engagement, shared how different departments are trying to help students during UCS’s restructuring.
“We all know what’s going on with UCS,” James said in a previous DePaulia post. “It’s not the only solution. This is part of what students are asking for and what we need to do.
Senior management has not issued a statement regarding UCS. During the fall term, Vice President of Student Affairs Gene Zdziarski sent a college-wide email about My SSP, but didn’t explain why they added the resource. President A. Gabriel Esteban did not address the lack of counselors in his 2021 State of the University presentation.
Provost Salma Ghanem said at the joint university town hall between staff, faculty council and SGA in January that they “will assess the situation as it unfolds”, according to previous reports from The DePaulia. She also said that they have no plans to invest more funds in UCS.
“Once the positions at UCS are filled, the university will assess whether the needs for mental health services have been met,” Ghanem told the meeting.
There have been no updates since then from the administration about UCS.
“The upper administration must be held accountable for the lack of support they gave to their students,” Reed said. “They didn’t address it because they think [My SSP is] working. They need to be held accountable by the students as a whole because it doesn’t work.
UCS was also present at the mental health fair. Yau said it was a way to be more in tune with students’ mental health requirements.
“These events have reinforced how important it is for us to be attuned to the diverse mental health needs of our students,” Yau said. “It will be helpful to listen to students and learn about gaps in support as well as the types of services that would support student success. »
Reed said she trusts Yau to lead UCS and implement new programs for students. This includes hiring various advisors.
“[Yau] said he really wanted a fairer approach to [counseling] and getting therapists who really represent the student body, whether it’s gay therapists or therapists of color, those who can communicate a little better with students,” Reed said.
UCS plans to implement group treatment programs for alcohol and drug use, trauma-informed care, and survivors of sexual violence in the fall of 2022.
 Roundtable participants meet via Zoom on Thursday evening. The opioid crisis is closer to home than many realize in Snohomish County, and the impacts are being felt throughout the community. It was one of the takeaways from Thursday night’s virtual opioid roundtable hosted by the Verdant Health Commission. Verdant Health Commission Chairman of the Board, […]]]>
Roundtable participants meet via Zoom on Thursday evening. The opioid crisis is closer to home than many realize in Snohomish County, and the impacts are being felt throughout the community. It was one of the takeaways from Thursday night’s virtual opioid roundtable hosted by the Verdant Health Commission. Verdant Health Commission Chairman of the Board, […]]]>
The opioid crisis is closer to home than many realize in Snohomish County, and the impacts are being felt throughout the community. It was one of the takeaways from Thursday night’s virtual opioid roundtable hosted by the Verdant Health Commission.
Verdant Health Commission Chairman of the Board, Jim Distelhorst, opened the meeting by sharing a 17 minute video on opioid use in Snohomish County, where overdose deaths have increased 20-30% since 2020. In 2020 alone, 525 Snohomish County residents died from opioid overdoses. Yakima County is the only other county in Washington with more opioid-related deaths.
Opioid use is not only harmful to users, it also harms other members of the community. For example, according to the Centers for Disease Control, one in three police officers will be stuck by a used needle during their career.
Verdant based in Lynnwood (find out more about how it works and how it is funded here) funds a range of health-related initiatives and has also launched its own Needle Service Program (SSP), Distelhorst explained. The needle exchange program provides drug users with sterile injecting equipment, safe disposal of needles, access to health care, treatment, testing and support.
Distelhorst pointed out that Verdant Health does not distribute free needles, which leads to more needles being improperly discarded.
“People only get the number of needles they give back,” Distelhorst said.
This helps limit the number of needles in the community and ensure that as many needles as possible are properly disposed of, he said.
Verdant has also addressed the opioid issue by hosting Narcan training. Narcan is a nasal spray that, when administered, blocks the effects of an opioid overdose. In January, Verdant partnered with Molina Healthcare and Snohomish County Social Services to host three training sessions attended by over 75 community members.
As a result, “there are now 75 more people in our community trained to recognize the signs of an overdose and administer Narcan,” Distelhorst said. “Each participant received a Narcan kit to take home. Each kit contains two Narcan nasal sprays. This means that there are now another 150 of these Narcan nasal sprays circulating in the community.
Verdant plans to hold additional Narcan training sessions in the coming months.
Roundtable speaker Linda Grant, CEO of Evergreen Recovery Center, said there is a stereotype that only teenagers use opioids, when in fact they don’t.
“We need to broaden our thinking about how we approach this,” Grant said. “About 70% of opioid-related deaths are people over 30.”
Evergreen’s naturopathic doctor, Andrew Dzikowski, said the clinic has seen a significant increase in relapses since the start of the COVID-19 pandemic. However, he added that Evergreen strives to be a place where patients feel they can come back if they need additional help.
“One of the things we strive for is that whether you’ve relapsed or not or are recovering, we want to be a safe place where people feel they can come back, whatever their situation. , without any judgement,” he said. “And that’s what we do. We create a safe and protected space for people to come at all stages of recovery and all stages of life and to guide them to a safer environment with housing, counselling, therapy, medical care and a warm, loving touch.
After the video, a Q&A session was held to answer questions from the community.
Many commenters have asked where teens can get drug treatments and access programs like SSP.
Distelhorst said the Center for Human Services offers outpatient treatment for teens. The center is a non-profit, community-based youth and family services agency that provides counseling and promotes drug and alcohol prevention. Northpoint Recovery, located in Bellevue, also offers treatment for children ages 12 to 17 and accepts Medicaid.
Grant said she empathizes with young people trying to seek help for addictions as resources have dwindled in recent years.
“The treatment of young people has just gone down terribly in terms of resources,” she said. “I know our legislature is trying to reinforce that this time, but the Center for Human Services is about it. Even the inpatient facility, Sundown M Ranch [located in Yakima] is the last hospital treatment center for young people. It’s just dying for no really good reason.
A commenter asked if facilities are experiencing longer stays than before due to the presence of drugs with stronger trace amounts.
According to Mishelle Rutherford, director of health services at Evergreen, the average stay for patients in rehab is five days. However, stays are getting longer as many drugs are now mixed with fentanyl, a synthetic opioid that is 80 to 100 times more potent than morphine. Because fentanyl takes so long to leave the body, patients experience withdrawal symptoms for longer periods of time.
“We find that it lives in the fat cells,” she said. “So he comes out at different times. So someone can feel better one day in rehab, and the next day they’re back in full withdrawal. It was really difficult to manage. »
Another commenter linked to this question, asking if it was proving difficult to convince insurance companies to cover longer stays.
Rutherford said Evergreen hasn’t had too many problems with insurance companies so far.
“As long as we can show there’s a medical need for them to be there,” she said. “This is where it gets tricky, because what we might consider a medical need in our detox field may not be exactly what the insurance company considers a medical need. So that poses problems. »
In fact, Rutherford said, there are more problems with patients leaving early.
“We end up having a lot of people leaving against medical advice around day four or day five because they don’t feel better,” she said. “So it’s kind of a complicated room just to get them through full detox. And of course going through rehab: that’s just the very beginning.”

Distelhorst ended the meeting by thanking the community for joining in and being open to learning more about the complicated processes of addiction treatment.
Any other questions or comments can be sent to Zoe Reese at [email protected].
— by Lauren Reichenbach
 CrossOver Healthcare Ministry recently announced that it was among 49 recipients to receive a grant from Direct Relief’s Fund for Health Equity, which mobilizes financial resources for organizations focused on non-clinical interventions that affect a person’s health. Commonly referred to as the social determinants of health, these factors include an individual’s physical, social, political, cultural […]]]>
CrossOver Healthcare Ministry recently announced that it was among 49 recipients to receive a grant from Direct Relief’s Fund for Health Equity, which mobilizes financial resources for organizations focused on non-clinical interventions that affect a person’s health. Commonly referred to as the social determinants of health, these factors include an individual’s physical, social, political, cultural […]]]>
CrossOver Healthcare Ministry recently announced that it was among 49 recipients to receive a grant from Direct Relief’s Fund for Health Equity, which mobilizes financial resources for organizations focused on non-clinical interventions that affect a person’s health. Commonly referred to as the social determinants of health, these factors include an individual’s physical, social, political, cultural and economic environment.
The 49 organizations received funding for a wide range of initiatives, including a campaign to overcome anti-Asian hostility and its effects on well-being; an initiative to develop more active lifestyles among members of the Yurok tribe; a center supporting the welfare of black women; and an organization focused on improving birth outcomes for refugee populations, primarily from African and Asian countries.
CrossOver was awarded a $250,000 grant from the Health Equity Fund for its work to provide high-quality, compassionate health services to low-income, uninsured, and medically underserved residents of the Greater Richmond area . CrossOver provides a medical home for patients, offering innovative integration of healthcare services under one roof, including primary and specialty care, chronic disease management, medication, dental, vision, pediatrics, counseling , women’s health and OB, HIV/AIDS diagnosis and treatment, case management and health education.
Each year, CrossOver provides care to more than 6,200 clients. CrossOver patients come from very different backgrounds: 80% of patients do not speak English as their first language, and more than 62% of all patients list Spanish as their primary language.
“This general operating support grant makes the work of CrossOver possible,” said Julie Bilodeau, CEO of CrossOver. “Quality healthcare requires excellence at every level: staff, facilities, programs, patient support and more. We are very grateful for Direct Relief’s support of our mission to provide health care to those in need.
“This round of funding honors the organizations on the front lines of their communities who are already working tirelessly to eliminate health disparities,” said Byron Scott, Health Equity Fund Co-Chair and Board Director. director of Direct Relief and chairman of its medical board. Advice. “These funds will allow these exemplary organizations to pursue innovation while improving health outcomes for vulnerable populations in diverse communities across our country.
The winners were selected by the Advisory Board of the Health Equity Fund.
Thanks for the reading!
If you enjoy our content, please consider making a monetary contribution to help us keep our news free.
Click here to contribute!
 This story is about suicide. If you or someone you know is at risk of suicide, please call the US National Suicide Prevention Lifeline at 800-273-8255, text HOME to 741741, or go to SpeakingOfSuicide.com/resources for resources additional. When the news broke that 22-year-old Stanford football star and senior Katie Meyer died by suicide last week, […]]]>
This story is about suicide. If you or someone you know is at risk of suicide, please call the US National Suicide Prevention Lifeline at 800-273-8255, text HOME to 741741, or go to SpeakingOfSuicide.com/resources for resources additional. When the news broke that 22-year-old Stanford football star and senior Katie Meyer died by suicide last week, […]]]>
This story is about suicide. If you or someone you know is at risk of suicide, please call the US National Suicide Prevention Lifeline at 800-273-8255, text HOME to 741741, or go to SpeakingOfSuicide.com/resources for resources additional.
When the news broke that 22-year-old Stanford football star and senior Katie Meyer died by suicide last week, it was a heartbreak to parents who understood what Katie’s mother, Gina, meant. , when she said she was having “a parent’s worst nightmare” in her interview with NBC News’ Stephanie Gosk on TODAY.
Especially terrifying for parents: Meyer told Gosk that she and Katie’s father had no red flags leading to his death and that she had been in good spirits on FaceTime with them hours before.
Katie’s death leaves questions about what parents need to know about mental health support on campus and how they can support their children in college, especially now that students seem to be struggling more than ever.
Related: Katie Meyer’s parents speak out after her death
According to the latest Healthy Minds Institute data report from Winter 2021, 41% of students surveyed reported moderate or major depression, and 13% said they had had suicidal thoughts in the past year.
We asked experts in the fields of mental health and higher education for their thoughts on what parents can do.
1. Start working on self-defense skills early
Think about the skills people need in college before your kids get into college, Myrna Hernández, vice president of student affairs at the College of Wooster in Ohio, told TODAY Parents. “While they’re still in high school, figure out what your child is dealing with, whether it’s academics, mental health, or anxiety,” she suggested.
“Then start building their self-advocacy skills,” she said. “Ask them, ‘What do you want to do about it and how are you going to achieve it? to be able to speak for themselves.
Read more: TODAY’s guide to young adults and mental health
2. Learn about mental health resources
When visiting college campuses, parents and students should ask about mental health services the same way they would ask about meal plans or internship opportunities, experts said — even if their students have never needed mental health support in the past.
Know who to contact in case of a problem. Know where the student health center is. Know how to find mental health help and make sure your college kids know too. At Wooster, for example, Hernández said the school has an “early warning system” in the form of a university “care team” made up of students, faculty and staff. staff who can follow up if someone alerts them with concerns about a student. .
Wooster offers counseling services through its Student Wellness Center, but Hernández noted that those services might have a wait time. She said Wooster and most colleges and universities also have emergency mental health support available 24 hours a day, seven days a week — which is important for students to know.
Other questions to ask colleges: How long do students typically wait to see a counselor? How many sessions are they given before they have to seek help outside of the university? What kind of support does the university provide if they need to find a private mental health provider?
3. Consider legal release forms
What many parents don’t realize is that once kids are over 18, privacy laws limit colleges in what they can tell parents about mental health. of their students.
In some cases, parents may want to submit documents signed by their students, which will give the college more freedom to tell them if their children are suffering from a medical condition on campus, whether mental or physical. These forms may include a medical and/or financial power of attorney as well as HIPAA authorizations.
“If a student welcomes this, it’s not a crazy thing to have, just in case,” said Dr. Sarah Cain Spannagel, licensed clinical psychologist and faculty member at Case Western Reserve University.
“My mom sent me off to college with a Tupperware with things like a little sewing kit in it,” Spannagel noted. “Did I use any of these things? No. They sat in a storage block in the corner of my dorm. But I had them if I needed them; and it’s really no different, if it makes sense to everyone involved.
4. Talk about mental health and have a plan
When a child goes off to college, the dynamic between them and their parents changes, Hernández said — and communication is important.
Once a student has been on campus for a few weeks, “Ask them, ‘Who besides your friends supports you?'” she said. “Make sure they can point to someone. Even a single connection, like a coach or a professor or someone from the academic resource center is enough, but they have to be connected to someone.”
For students who received mental health support in their hometown, a “direct continuity of care plan” is also essential, Spannagel said, and not just in terms of counseling or medication.
“Whatever personal care your child takes at home, it has to accompany them in some way through college,” she said. “If they have a gym membership at home and working out helps relieve their stress, make sure they know where they can do it on campus. nails every week, so they should.”
5. Work on noticing instead of judging
Spannagel advised parents to stay in regular contact with their kids in college and insist, sometimes, on hearing their voices or FaceTiming so they can see what they look like. However, she warned that parents should be “observers” when watching their children and not judge them.
If they are grumpy from lack of sleep or not eating enough, instead of criticizing them, be aware and notice if a child seems to be eating, exercising or sleeping more or less than usual, has she declared. Significant changes can be an early warning signal that something is wrong. A big say a student might need help with, Spnagel said: any mention of desperation.
Spnagel also said that while students need their independence, it’s okay for parents to decide to take something off their child’s plate.
“If you have to pick up their medicine from the pharmacy and mail it to them at school, who cares? ” she says. “There are a million other opportunities in college to be independent. If they need you to do that one thing to keep them on track, that’s OK.”
6. Tell your kids they’re not alone if they’re struggling
Samantha Arsenault Livingstone is an Olympic swimming gold medalist who battled depression and now works as an educator and mental health advocate. She knows all too well the perfectionism and pressure that Katie Meyer’s parents mentioned in their TODAY interview, for both top athletes and the average person.
Going to college as an elite athlete, she would have benefited from knowing that “other people struggled as well,” she told TODAY Parents. “I completely believed that I was the only one. Even after all my achievement, I felt like an impostor, and that for me was the driver into the depths of depression, into this dark, dark space, because I had felt like I would be found out if I revealed some kind of struggle.
Livingstone noted, “We don’t need a diagnosis to be able to talk about anxiety. Sometimes children feel they need permission to feel what they feel.”
Hernández said the mental health crisis among students is “generational,” not just a byproduct of the COVID-19 pandemic.
“We must remember that it is getting worse now, as not only are students dealing with the disruption caused by the pandemic, but they have also grown up in schools with the anxiety and stress of active shooting drills and thinking to their personal safety every day just at school in general,” she said.
Related:
 BELFAST, Maine — A girl who a Sweetser employee allegedly sexually assaulted while the teenager was living in Belfast’s residential treatment center is suing the nonprofit for negligence, negligent supervision and more. The teenager, identified as “Jane Doe”, and her mother are also suing former Sweetser employee Trey Knof. The 25-year-old from Newcastle is currently […]]]>
BELFAST, Maine — A girl who a Sweetser employee allegedly sexually assaulted while the teenager was living in Belfast’s residential treatment center is suing the nonprofit for negligence, negligent supervision and more. The teenager, identified as “Jane Doe”, and her mother are also suing former Sweetser employee Trey Knof. The 25-year-old from Newcastle is currently […]]]>
BELFAST, Maine — A girl who a Sweetser employee allegedly sexually assaulted while the teenager was living in Belfast’s residential treatment center is suing the nonprofit for negligence, negligent supervision and more.
The teenager, identified as “Jane Doe”, and her mother are also suing former Sweetser employee Trey Knof. The 25-year-old from Newcastle is currently in jail awaiting trial on several counts, including unlawful sexual touching of a minor, aggravated sexual assault, breach of bail conditions and possession of sexually explicit material.
The lawsuit alleges that Knof sexually assaulted the girl, even after Sweetser fired him, and that Sweetser failed to take appropriate action after learning of the employee’s behavior.
The teenager was admitted to Sweetser’s residential treatment program in Belfast in December 2018 when she was 13. Agency officials knew she had suffered multiple sexual assaults as a child and needed specialist treatment and protective precautions, according to the complaint filed by her lawyer, Stephen Smith. of Augustus.
Nonetheless, the company hired Knof as a caregiver in January 2019 and failed to conduct an adequate background check, according to the lawsuit, filed earlier this month in Somerset County Superior Court.
“Knof had no prior experience and no special training to be a counselor or caregiver,” the lawsuit said. “Knof’s only qualification to work at Sweetser seemed to be that he had worked as a veterinary assistant at an animal hospital.”
Knof was assigned to the girl’s unit, where despite a lack of training in maintaining boundaries or dealing appropriately with young girls with traumatic histories, his job was to drive the teen and other residents to appointments. and to provide emotional support, according to the lawsuit.
Knof “began having an inappropriate relationship” with the girl in the summer of 2019, according to the lawsuit. In June, the teenager told emergency department staff at Waldo County General Hospital, where she was taken for a crisis assessment, that she believed she was pregnant and had had unprotected sex the previous week.
A few days later, she was taken 200 miles north to the Children’s Crisis Unit at Aroostook Mental Health Services in Fort Fairfield. Knof visited her there, sat her on his lap and was seen touching her inappropriately, according to the lawsuit.
“During this visit, Knof told the plaintiff, ‘We can date secretly until you’re older, because if anyone finds out, I could get in legal trouble,’ the lawsuit said.
The crisis unit director called Sweetser after learning about Knof’s visit. Aroostook County staff also notified the girl’s mother, identified as Mary Doe in the lawsuit.
But Sweetser officials and staff never asked the girl about Knof’s visit or informed her mother. When her mother brought it up with Sweetser staff at a meeting that month, the Belfast living unit supervisor told her it was “dealt with,” according to the lawsuit.
Knof made special visits to the girls’ unit weekly, and sometimes daily, just to see her, according to the lawsuit. He would also take bets with colleagues on “who could sleep with the plaintiff first,” according to the lawsuit. Also, when Sweetser’s staff thought the teen needed to be disciplined, they had Knof restrain her by having her sit on his lap while he hugged her tightly.
“This ‘discipline’ was practiced frequently by Knof,” the lawsuit said.
Sweetser held multiple counseling sessions with Knof over several months regarding “breaking boundaries” with the girl, and at one point the agency tipped him off and asked him not to go to his unity.
But in December 2019, Knof entered the girl’s bedroom and sexually assaulted her, leaving behind a bag of Skittles, “as if for payment”, according to the lawsuit. About an hour later, another employee asked the girl why Knof came and how the girl got the candy. But Sweetser never addressed the incident, according to the lawsuit.
Knof was fired on January 3, 2020, but the agency did not tell the girl’s mother or take any further precautions. A few days later, the unsupervised teenager met Knof in the parking lot of the Hutchinson Center at the University of Maine in Belfast, where he sexually assaulted and abused her in his vehicle, according to the lawsuit.
The teenager spent the following weekend at her mother’s home in Somerset County, and while she was there Knof snuck into her bedroom window and sexually assaulted her, the lawsuit alleges . Knof also told the teenager that he still had a set of keys for Sweetser, then made a plan to run away with her to another state.
On January 13, someone found a tablet at the residential center in Belfast which contained messages between Knof and the girl, including explicit photos and sex memes. A sex toy was also found in the girl’s bedroom, along with a handwritten, sexually explicit letter that read “From Trey” at the top.
Sweetser eventually informed the girl’s mother of Knof’s abuse and reported it to the Belfast Police Department that day, according to the lawsuit. Three days later, detectives spoke to the girl, who said she had frequent sex with Knof, and the two were “constantly talking” via social media.
But she told police Sweetser’s staff didn’t notice her because she was “invisible to them,” according to the lawsuit.
After Knof was arrested and charged in connection with the alleged sexual abuse, the girl tried to process her feelings about what happened with other Sweetser staffers.
“Instead of listening to plaintiff with support and understanding, Sweetser staff threatened plaintiff with punishment for discussing these events,” the lawsuit said.
But Sweetser staff told her colleagues and other residents about Knof, so the girl was harassed by other residents.
The lawsuit seeks to find Sweetser liable for negligence, negligent supervision, invasion of privacy and negligent infliction of emotional distress. He also seeks to find Knof liable for sexual assault and battery and intentionally inflicting emotional distress.
Plaintiffs are seeking unspecified damages, costs, and attorneys’ fees from both Sweetser and Knof.
Justin Chenette, director of communications and public relations at Sweetser, said the agency could not comment on the lawsuit at this time.
“The well-being of the customers we serve is our top priority,” he said.
Jeremy Pratt of Camden, a defense attorney representing Knof on the criminal charges but not the civil case, said Thursday he had no comment.
More articles from the BDN
 by LF In the request made by the Regions, it is requested that a passage be included in the law on which the Ministry of Health is working to allow the “recruitment of employees to guarantee the primary care activities to be carried out within the homes of the community”. But the negotiation with the […]]]>
by LF In the request made by the Regions, it is requested that a passage be included in the law on which the Ministry of Health is working to allow the “recruitment of employees to guarantee the primary care activities to be carried out within the homes of the community”. But the negotiation with the […]]]>
by LF
In the request made by the Regions, it is requested that a passage be included in the law on which the Ministry of Health is working to allow the “recruitment of employees to guarantee the primary care activities to be carried out within the homes of the community”. But the negotiation with the government is not yet unblocked. The crux of the clause which would allow the ministry to intervene if the negotiations with the MMG of Sisac could not succeed.
February 11th – “The Regions and Autonomous Provinces, through the organs of the regional health service, can recruit employees to guarantee the primary care activities to be carried out within the homes of the community, within the current limits of personnel expenditure accumulated with the final expenses as at 31.12.2021 for the purchase of health services for basic medicine“.
This is the request put in black on white by the Regions and transmitted to the Government so that this approach is included in the measure of reorganization of territorial medicine on which the Ministry of Health is working. In essence, the regions ask that, alongside the figure of the contracted family doctor, they can be hired as employees of the doctors to work in the houses of the community.
At the moment, however, negotiations are still at a standstill and what the minister is learning Hope he would not have much appreciated the request to open up the possibility of hiring dependent doctors in the Community Houses.
As we have already written in recent weeks, however, the pressure, especially from the Campania region, is strong, which also complains that the whole issue of the dispute does not fall within the competence of the national government and is contrary to the intention to include in the law a replacement intervention of the minister in charge of health in the event of disagreement with the general practitioners within Sisac to define the agreement.
A point on which also Veneto, the public administration of Bolzano and also Puglia seem to converge which denounces as the new role proposal for mmg (weekly schedule of 38 hours and more or less half in the study and half in community houses and district services) does not substantially alter the status quo.
On the other hand (Lombardy, Piedmont, Emilia-Romagna and Sardinia in particular), if they do not entirely agree with the ministerial proposal, they think rather that an agreement must be reached in order not to risk losing the resources of the PNR (7 billion for the territory) and that in any case, if this is the case, this proposal nevertheless represents a good starting point to reverse the status quo.
LF
February 11, 2022
© All rights reserved
Other articles in Trades and Professions






Online news
health information.
QS Edizioni srl
VAT number 12298601001
Via Boncompagni, 16
00187 – Rome
Via Vittore Carpaccio, 18
00147 Roma (RM)
Cesare Fassari
Managing Editor
Francesco Maria Avitto
President and CEO
Vincenzo Coluccia
General manager
Ernesto Rodriquez
Copyright 2013 © QS Edizioni srl. All rights reserved
– VAT number 12298601001
– registration in the ROC n. 23387
– registration at the Court of Rome n. 115/3013 of 05/22/2013
All rights reserved.
Privacy Policy
 After the earthquake, the families of Chardonnières are barely recovering. By Moliere Adely Six months after the earthquake that shook Haiti on August 14, 2021 – killing nearly 2,200 people, injuring 12,700 and affecting around half a million children – UNICEF continues to help families, and by especially children, who were the main victims. In […]]]>
After the earthquake, the families of Chardonnières are barely recovering. By Moliere Adely Six months after the earthquake that shook Haiti on August 14, 2021 – killing nearly 2,200 people, injuring 12,700 and affecting around half a million children – UNICEF continues to help families, and by especially children, who were the main victims. In […]]]>
After the earthquake, the families of Chardonnières are barely recovering.
By Moliere Adely
Six months after the earthquake that shook Haiti on August 14, 2021 – killing nearly 2,200 people, injuring 12,700 and affecting around half a million children – UNICEF continues to help families, and by especially children, who were the main victims. In Chardonnières, with the support of UNICEF, dozens of families are receiving training in health and nutrition to improve the care of their children.
Chardonnières, Haiti, February 14, 2022 – At only nine months old, Syndia Célestin experienced the greatest pain: her mother died after fighting for her life for several months. The August 14, 2021 earthquake found her bedridden in her mother’s house in Chardonnières unable to move to seek shelter. Debris fell on his legs and his health deteriorated despite receiving medical attention. Her newborn daughter needed urgent help to survive. Her grandmother, Vita Lubin, 53, welcomed her into her home to offer her food, a home and a loving embrace.
The girl’s mother was ill for months before she died in late December. “I took her to several hospitals. I sold almost everything I had to get the money for her medical treatment. Unfortunately, we couldn’t save her,” says Vita, sitting on the terrace of his house, visibly damaged by the earthquake. , as desolation permeates its history.
In addition to being motherless, Syndia Célestin suffers from severe acute malnutrition. Despite her best efforts, Vita lacks the resources to meet her granddaughter’s food and care needs. “I feed him whenever I can. Some days I just give him bread and peanut butter, but that’s not enough,” she laments. Her job as a food vendor is not enough to make ends meet and her savings disappeared between the earthquake and her daughter’s illness. She now lives in a poor neighborhood of Chardonnières with the baby and other family members.
As in the rest of the municipalities of southern Haiti, the earthquake destroyed or damaged a large part of the houses and buildings of Chardonnières. Many families have been left homeless, facing uncertainty, food shortages and lack of access to the most basic services, including drinking water.
Changing habits and increasing child malnutrition
Eveline Dominique Chery, health officer for UNICEF in Les Cayes, believes that the earthquake has completely changed the lives of the inhabitants of the southern coast of Haiti. Families have been forced to change their diet: “It has become very difficult for people to access the food they used to eat. Some families even reduced the number of daily meals they gave their children; others have changed the way they cook. very strong impact on the nutrition of children in Chardonnières,” she explains. Six months later, the situation has hardly changed.
UNICEF estimates that nearly half a million children have been affected by the earthquake, with little or no access to shelter, clean water, medical care and nutrition. “The overall rate of acute malnutrition at the national level is 6%. In the south it is 4.7%, but this figure probably increased after the earthquake,” says Eveline.
The Communion of Mothers
Odena Michel, 46, is a mother of two children and a volunteer collaborator (Col-vol) at the Club des Parents de la Bousquette – a village in the Chardonnières – which meets once a month in a church. “In 2011, I started training mothers and organized several groups. I prepare hygiene and nutrition training activities, cooking demonstrations, and also examine girls and boys in the club” , explains Odena, who trained as a community health worker. Vita Lubin is one of the club’s members and a committed grandmother who regularly attends club meetings to improve the present and future life of her granddaughter, Syndia Célestin.
Mantoute Marie Rolande is a nurse at the Sainte Anne Health Center in Chardonnières, and one of the people who manages the nutrition and vaccination services for children. “In recent months, we have detected malnutrition in more than ten children,” she says. On February 1, 2022, she welcomed Syndia Célestin to the hospital, who passed a health check for the first time since her birth. After examining her, Mantoute provided the baby with several doses of vaccines and gave her grandmother Plumpy’Nut to continue feeding her at home. Plumpy’Nut is a ready-to-use therapeutic food based on peanut paste and easy to administer for the treatment of severe acute malnutrition.
The Parenting Club had ceased operations after the earthquake, but slowly resumed meetings. The objective is to mobilize women to improve the nutritional situation of children in the area. “Thanks to the Parenting Club, in recent years there have been fewer malnourished children in the region,” explains Col-vol Odena.
There are currently 179 clubs operating in the Grand Sud region and although these groups have been around for years, they are proliferating thanks to UNICEF support to the Ministry of Health.
“UNICEF, through the Integrated Health Services for Adolescents and Women (SSIAF) project, cooperated with the Ministry in the training of ASCPs (Multipurpose Community Health Workers). It also helps us with the clubs, by supporting the activities that the mothers organize each month”, indicates Céline Percy Élysée, Child Health Coordinator at the Direction de la Santé du Sud. The SSIAF project is funded by Canada and implemented by UNFPA, UNAIDS, PAHO, WHO and UNICEF.
Wilnèse Mogène, 31, lives with her daughter in Lapas 2, a village in the Chardonnières. In 2016, she was invited by Odena to join the club. “Thanks to the Parenting Club, I learned a lot of things. They taught me the principles of hygiene and nutrition. I learned to balance what you eat at home,” she says. The training she received at the club enabled her to better feed her 10-year-old daughter. “Before, my daughter often had headaches. She did not understand what she was studying. Since I started serving her balanced meals, she no longer has headaches. Now she is studying well and remembers all the lessons,” says Wilnèse.
Her daughter, Wiltana-Beaudier St-Cyr, a CM2 student, lives with her, but was on vacation with her father when the earth shook on August 14. “I immediately thought of my mother. I was scared,” Wiltana recalls. She says she is always scared when there are earthquakes because she knows that when the earth shakes she might be one of the victims. This underlying fear does not, however, prevent her from dreaming about her future: “When I grow up, I want to be a nurse to care for the sick.
Since the earthquake, UNICEF and the Ministry of Health have tested 21,800 children under five for acute malnutrition. More than 1,100 children among them were treated for acute malnutrition and 3,700 for moderate acute malnutrition. UNICEF has pre-positioned emergency nutritional supplies to care for 27,000 children suffering from acute malnutrition in Nippes, Sud and Grand’Anse affected by the earthquake.
 Many people who live in rural Appalachia struggle to access reliable internet, so they may not be … [+] able to video chat with a doctor or therapist. Getty Late last year, on November 19, the House of Representatives passed Biden’s Build Back Better infrastructure plan. Of these funds, $475 million will go to the […]]]>
Many people who live in rural Appalachia struggle to access reliable internet, so they may not be … [+] able to video chat with a doctor or therapist. Getty Late last year, on November 19, the House of Representatives passed Biden’s Build Back Better infrastructure plan. Of these funds, $475 million will go to the […]]]>
Many people who live in rural Appalachia struggle to access reliable internet, so they may not be … [+]
Getty
Late last year, on November 19, the House of Representatives passed Biden’s Build Back Better infrastructure plan.
Of these funds, $475 million will go to the Connected Device Grant Program to distribute tablets and computers to those in need. An additional $2 billion will support USDA’s ReConnect program, which will improve broadband access in rural communities.
In 2022, advocates anticipate these infrastructure changes will slowly begin to roll out across the United States. The road to better health care in Appalachia is a tough journey, but broadband access could be a revolutionary first step.
How Rural Infrastructure Affects Health Care
When you imagine infrastructure, you probably think of roads, bridges and architecture. But the infrastructure also includes doctors’ surgeries, affordable internet access and other tools that help people connect to essential services.
Appalachia struggles with great inequities in infrastructure, and these disparities impact how rural residents may or may not receive the health care they need. There are far fewer medical professionals working in Appalachia than in other parts of the country. In 2019, the Appalachian Regional Commission released a survey to estimate the number of primary care providers and mental health professionals working in the region per 100,000 patients. With 35% fewer mental health care providers than the national average, Appalachia has few options for counseling or psychiatric services. In some mountain communities, patients must travel for hours to reach their nearest therapist or medical specialist. Travel can be difficult if these patients do not have public transport or have to drive on broken roads.
Patients do not have easy access to mental health services, but the demand for care is overwhelming. Appalachia report high rates of mental illnesses like depression, anxiety, suicidal thoughts, and they are also at risk for developing chronic diseases like diabetes and cancer. Robert Bossarte, PhD, is the principal investigator of the Appalachian Mind Health Initiative. Bossarte explains how rural infrastructure has left many patients behind: “We have to recognize that there is a national shortage of healthcare providers. And because West Virginia is an under-resourced market, there aren’t many vendors here. With months-long waits for doctor appointments and advice, it can feel like a race against time to sort out patients who need help.
Annsley Roberts was one of the patients involved. Roberts grew up in western North Carolina, where there is a mental health center throughout her county. She tried to get counseling for coping with depression after her father’s death, but Roberts had few options: “The only mental health center near me is so busy it often pushes its patients to join group therapy. I have had friends who have stopped going to therapy altogether because they were pressured to attend group sessions. Group sessions can provide valuable support to patients. But Annsley was all too aware of how gossip can spread in a small town, and she feared revealing personal (and vulnerable) information in a group setting. She, like some of her friends, felt they needed confidential, individual sessions with a therapist.
Patients who do not have access to mental health care often turn to their primary care physician for help. However, most GPs do not have the specialist training to serve as makeshift therapists or psychiatrists. Going to see his doctor helped Roberts cope in the short term, but it was ultimately a band-aid solution. “I ended up seeing my GP. Although she may have gotten me started on medication, I still feel that I would have benefited greatly from a combination of medication and therapy,” Roberts says.
How Biden’s infrastructure plan could expand telehealth options
With these infrastructural obstacles, patients like Annsley Roberts can feel stranded. Technological barriers can make patients even more isolated. “I wish I could connect with a therapist via computer, but getting a reliable internet connection is difficult,” Roberts says. She is not alone. A survey by SSRS and the Bipartisan Policy Center found that 45% of people living in rural communities report technological issues such as spotty Wi-Fi signal as a barrier to accessing telehealth.
Expanding broadband access in Appalachia could help patients access more telehealth options, right from home. Looking ahead to 2022, health advocates hope Biden’s plan will provide federal broadband rebates for low-income families and invest federal funds in expanding internet service in areas that are currently not covered. Some healthcare professionals say telehealth is the next step in healthcare in an increasingly digital world. “The healthcare industry is moving towards monitoring systems, patient self-monitoring, computer-assisted therapy and instructional videos. Results from surveys of residents of many states have indicated that 80% of Americans use the Internet for mental health information,” the researchers explain in an article published in the journal. Acta Informatica Medica. Several medical studies have shown that telemental cognitive behavioral therapy can reduce a patient’s feelings of loneliness, anxiety, and depression.
Physicians already using telehealth in rural areas of America have reported significant positive results. 20% of patients in the SSRS and Bipartisan Policy Center survey said they would have delayed or avoided a medical appointment if they had not been able to schedule a telehealth appointment. Fortunately, 80% of these patients said their telehealth appointment was successful in resolving their health issues. 94% of respondents were satisfied with the quality of care received during their telehealth appointment. Robert Bossarte also observed these positive benefits in Appalachia. “Here, physicians using telehealth have seen fewer missed appointments.” Currently, Bossarte’s team of mental health professionals must use a variety of approaches to reach patients who do not have reliable internet. The Appalachian Mind Health Initiative schedules appointments by phone and video chat, depending on the patient’s technology access. But some patients may benefit from the ability to use videoconferencing. In a study published in Oncology time, 72% of patients preferred to communicate with their doctor face to face. Many patients find telephone or text communication to be impersonal. Other patients may appreciate being able to see their doctor’s body language. Biden’s broadband plan can help these patients have a stronger connection with Zoom and with their doctors.
Despite Bossarte’s best efforts, he knows broadband access will be a victory in a larger war for rural health care access. Some Appalachian practitioners are hesitant to embrace telehealth. “When we started the Appalachian Mind Health Initiative, we had over 100 clinicians saying, ‘Yeah, we’re really happy to work with you. But when it comes to adopting these new approaches, only a handful of these practitioners follow,” says Bossarte. These uncertain practitioners can draw inspiration from some data on the effectiveness of telehealth. For example, the Community Mental Health Association of Michigan reported that ⅔ of behavioral health providers used telehealth in 2021. 60% of these providers used videoconferencing with their patients, and 68% of physicians noted that telehealth increased satisfaction and retention of their patients. . Of these practitioners, 74% plan to permanently offer telehealth options (including video chat appointments) after the Covid-19 pandemic.
Broadband will not automatically improve Appalachian health outcomes. Biden’s infrastructure plan is no panacea for the region’s deep health infrastructure inequities. However, Biden’s proposal to expand internet access may remove a stumbling block for health care. “Times are changing. There is hope. I think about how telehealth would have helped me, and I hope this technology can help future people connect to the healthcare they need” , says Annsley Roberts.
Telehealth can help struggling patients realize they are not alone, even if they live miles from a doctor’s office.
 Transgender employees and dependents can now access gender-affirming care and medical management services Annapolis, MD (January 28, 2021) – Anne Arundel County Manager Steuart Pittman today announced that new Anne Arundel County employee health benefits, offered through Aetna, will include gender-affirming healthcare for employees and dependents. The new employee medical benefits went into effect on […]]]>
Transgender employees and dependents can now access gender-affirming care and medical management services Annapolis, MD (January 28, 2021) – Anne Arundel County Manager Steuart Pittman today announced that new Anne Arundel County employee health benefits, offered through Aetna, will include gender-affirming healthcare for employees and dependents. The new employee medical benefits went into effect on […]]]>
Transgender employees and dependents can now access gender-affirming care and medical management services
Annapolis, MD (January 28, 2021) – Anne Arundel County Manager Steuart Pittman today announced that new Anne Arundel County employee health benefits, offered through Aetna, will include gender-affirming healthcare for employees and dependents. The new employee medical benefits went into effect on January 1, 2022 after internal announcements and employee briefings.
“Providing our LGBTQ+ employees and residents with the support they need is essential to our mission to make Anne Arundel County the best place for everyone,” said County Executive Steuart Pittman. “Now our employees and their families will have access to the care they need to live freely as they are.”
Joe Toolan, President of Annapolis Pride, said, “We are grateful to the county executive for their leadership in transgender and transition health care. Lawmakers in 32 states are actively blocking or failing to provide this essential medical care. Research demonstrates that gender-affirming care designed to affirm individuals’ gender identity significantly improves the mental health and overall well-being of gender-diverse, transgender, and non-binary people. The reality is that gender-affirming healthcare saves lives and we are proud of this major victory for our county employees.
Anne Arundel County Medical Benefits supports gender-affirming medical management services, including pre-certification, care management, and behavioral health services. When someone needs gender-affirming surgery, Aetna performs reviews of the medical necessity and benefits of the procedure, and assists them with care management and patient support before and after surgery. They also have a clinical pharmacist on their care team who can help with questions about hormone therapy medications.
“Access to gender-affirming medical care is an essential part of health insurance benefits for transgender people,” said Abbie Ellicot, President of WISE LGBTQ+ Advocacy Huddle. “We commend the County Executive and its administration for including these important employee benefits and for continuing the important work around diversity, equity and inclusion.”
Through the blanket, participants can receive education on their transition options and ongoing emotional and mental support. Employees can also be referred to counseling, local behavioral health program support groups and online resources.
“These new medical benefits will help ensure that we meet the health coverage needs of all of our staff,” said Anne Budowski, Director of People.
Employees who have questions or need more information about gender affirmation services offered through their county medical benefits should visit aacounty.aetna.com or contact Aetna Member Services at 1-855 -222-2774.
 Senior Pastor Willie Davis and his wife, Pastor Ciara Davis, founded Invisible Reality Ministries in their home in 2011. (Photo by Matt Martinez) For the Davis family, Sunday mornings have always been hectic. At first Reverend Willie Davis woke up and slid the dining room table into the laundry room. His wife, Ciara, joked that […]]]>
Senior Pastor Willie Davis and his wife, Pastor Ciara Davis, founded Invisible Reality Ministries in their home in 2011. (Photo by Matt Martinez) For the Davis family, Sunday mornings have always been hectic. At first Reverend Willie Davis woke up and slid the dining room table into the laundry room. His wife, Ciara, joked that […]]]>
Senior Pastor Willie Davis and his wife, Pastor Ciara Davis, founded Invisible Reality Ministries in their home in 2011. (Photo by Matt Martinez)
For the Davis family, Sunday mornings have always been hectic.
At first Reverend Willie Davis woke up and slid the dining room table into the laundry room. His wife, Ciara, joked that she needed a new table after all the wear and tear. But they had to make room for him to have a place to preach.
Soon people began to flock. Eventually they moved to the Dineen Park Pavilion. And then they rented space at Mount Mary University.
It took years to find the place where they would build their church, and even more to settle there. But Willie and Ciara never lost faith. They were on a mission.
Unseen Reality Ministries, 2700 N. 54and St., is a non-denominational Christian church. Willie is senior pastor and Ciara is a fellow pastor. Their three daughters – Destiny, Ashanti and Trinity – are also involved in the church.
“That’s what really defines us,” Willie said. “That’s our goal. That’s why we’ve been through what we’ve been through throughout our lives.
Willie and Ciara, both Milwaukee natives, see their church as the best way to give back to the communities where they grew up.
Invisible Reality has engaged in initiatives to promote health for its congregation, including a partnership with the Medical College of Wisconsin that led to implicit bias trainings and advocacy for black and brown patients in a ward of examination.
Jeff Morzinski, professor emeritus at the Medical College of Wisconsin, said Willie’s work with MCW has evolved over the years from youth outreach to work in rehabilitation programs for incarcerated people. Back to school in particular, Morzinski said, was one area where Willie brought a holistic approach.
“He knew people needed personal support,” Morzinksi said. “He knew how to build forgiveness and connect with his own neighborhoods and community.”
The church also hosts the HEALTH program, an acronym for “helping everyone achieve a healthy life.” The program connects church members with Alverno College graduate students who can provide free consultations and help identify medical issues.
Ministry of Mental Health
Additionally, the church provides free mental health services.
Every Wednesday, the church hosts Stronghold sessions from 5:30 p.m. to 7 p.m. Group discussions bring congregation members seeking help with addiction and depression together and connect them with pastors and Jim Gerber, a psychotherapist.
Ciara said the idea is to give people psychological help and spiritual support. Free services are intended to help those who need help but otherwise could not afford it.
“Jesus and therapy will meet the need,” Ciara said. “You need both.”
Willie said the sessions have helped people overcome addiction, anxiety and suicidal thoughts.
Gerber said Invisible Reality stands out from other bands he has worked with because of its commitment to the community. The people in the program look out for each other.
“People move forward in groups,” Gerber said. “It makes a significant difference – they’re not as isolated.”
A vision for the community
Willie grew up surrounded by gangs, drugs and violence. When he needed a safe space, he had his grandmother’s house.
“My upbringing was very tough. If it hadn’t been for my grandmother, I don’t know if I would even be here today,” he said.
Willie was born and raised on North 23rd and West Lloyd Streets, near the Amani district. His grandmother, who acted as the “mayor” of the neighborhood, was also the woman who taught him everything he now knows about faith.
“She validated every aspect of the Word for me,” Willie said. “The love I have for community, the love I have for family, my understanding of what family should be like – I got that from my grandmother.”
And he wants others to have the same experience.
“It has to be something better,” Willie said. “A neighborhood that is hurting and full of violence, drugs and gang activity – there’s no way that’s the norm. There’s no way that’s the accepted rule.
The church tried to make this “something better” a reality.
Invisible Reality Ministries is a member of Common Ground, a grassroots group in southeastern Wisconsin working to address social issues. Willie recently worked with the group to try to reduce gun violence.
The church also runs other initiatives, including periodic soup kitchens, back-to-school fairs, and youth programs.
“To see families come in and they’re excited and their lives have been changed, and they’re starting to see their purpose and believe that they could be better off in life,” Willie said. “It’s worth it for us.”